×
Craniotomy/Brain Tumour Excision Surgery in India
What is brain tumour?
A brain tumour is an abnormal growth of tissue in the brain. This abnormal growth is the consequence of the uncontrolled multiplication of certain cells in the brain. As these cells multiply progressively, the tumour emerges. Broadly speaking, there are two kinds of tumours:
Benign Brain Tumours: These tumours are slow-growing and restrict themselves to the brain, that this, they do not migrate to other parts of the body. However even this category of tumours may need to be removed if the growing mass affects proximate healthy tissue, increases the pressure within the brain and otherwise affects the functioning of this vital organ. Some of the common benign brain tumours are: pituitary adenoma, craniopharyngioma, meningiomas, neurocytoma, epidermoid cysts, haemangioma, etc
Malignant Brain Tumours: These tumours grow much faster than benign brain tumours. Primary brain tumours, which originate within the brain, may also metastasise (spread) to other parts of the body. Some examples of the common malignant brain tumours are: High Grade Astrocytoma/Glioma, lymphoma, ependymoma, medulloblastoma, etc
Most brain tumours, however, have their origin in primary tumours that originate in other parts of the body such as the liver, the breast, etc.
Craniotomy/Brain Tumour Excision Surgery in India
If the neurologist and the neurosurgeon decide that a brain tumour, benign or malignant, needs to be treated, the most likely approach is surgery.
The surgery for removal of a tumour in the brain is called craniotomy. The surgery is mostly done under general anaesthesia, except in those situations where brain mapping-which requires the inputs of the patient during the surgery-is involved. Brain tumour excision surgery can take several hours. A great amount of planning happens prior to the brain surgery in India with extensive use of imaging techniques.
What happens during Craniotomy/Brain Tumour Excision Surgery in India:
Under general anaesthesia, the surgeon makes an incision along the planned line, exposes the skull and uses a special tool to cut away a section of the skull. The objective of the surgery would be the total removal of the tumour. However in many cases, the surgeon may be compelled to limit the excision in order to avoid damage to surrounding healthy tissue and compromising on brain function. This situation happens when the tumour is in an inaccessible part of the brain. In extreme cases, the surgeon may also have to be content with removing a small portion of the tumour for pathological analysis. In all cases, it is standard practice to send tumour tissue for a biopsy. The objective of such analysis is to obtain an understanding of the specific nature of the tumour, so that subsequent treatment by way of chemotherapy or radiotherapy can be appropriately targeted.
In some cases of malignant tumours, the surgeon may also decide to deploy polymer chips at the tumour site in order to achieve concentrated local delivery of chemotherapy.
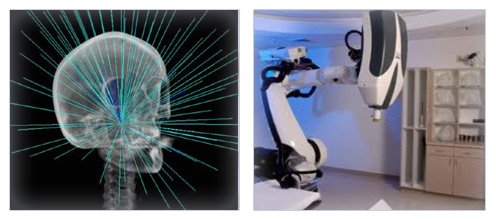
High-tech imaging in Brain Surgery in India
Leading hospitals in India use extremely sophisticated surgery navigation. The sophisticated imaging and mapping technology enables a very close identification of tumour location. This facilitates very precise planning of the incision to avoid/minimise trauma to healthy brain tissue in the course of the surgery. The objective is also to maximise tumour removal to the extent possible. Stereotactic techniques, wherein imaging is done using 3-axis, also allows for a very high degree of precision while planning treatment.
Hospital stay following brain surgery in India:
Patients would normally need to stay in hospital for about a week following craniotomy It is usual for patients to spend at least a day or two in ICU for monitoring vitals before they shift to standard rooms for recuperation.
Supplementary lines of treatment:
If complete excision of a malignant tumour was not possible during surgery, it may be necessary for the patient to also undergo chemotherapy or radiotherapy.
×
Minimally Invasive Endoscopic Neurosurgery in India
What is minimally invasive endoscopic neurosurgery?
Revolutionary technology has today made it possible for even complex brain surgeries to be carried out in a minimally invasive manner. In the past open surgery was the norm for carrying out brain related procedures. Typically, in order to remove a 3 cm tumour, the surgeon would make a 10 cm incision.
The development of the neuro endoscope has changed the way brain surgeries can be done. The neuro endoscope uses a video camera and micro-surgical instruments mounted on the tip of a flexible tube which can be maneouvred through complex body and brain anatomy. The endoscope can be as small as 2.7 mm, and the skin incision can be tiny - as small as that of a small coin.

The video camera provides the brain surgeon with an absolutely clear and well lit image of the inside of the brain on a magnified screen. The result is that the neurosurgeon is able to visualise brain tissue extremely clearly and is able to distinguish between normal tissue and abnormal or cancerous tissue. This enables the complete removal of abnormal tissue and the sparing of healthy tissue, leading to preservation of brain function and minimisation of collateral damage during brain surgery in India.
Which are the brain surgeries that are being done using endoscopic neurosurgery?
Advances in neuroendoscopic surgery have today made it possible to perform several brain surgeries in India in a minimally invasive manner:
- Acoustic neuromas
- Meningiomas
- Arachnoid cysts,
- Trigeminal neuralgia
- Craniopharyngiomas
- Pineal tumors
- Colloid cyst removal
- Neurocysticercosis
- Spine surgeries:
- thoracic disc removal
- lumbar disc removal
- Hyperhidrosis
- Upper limb sympathetic mediated pain.
- Hemifacial spasm
Procedures related to Hydrocephalus:
- Aqueductoplasty
- Third ventriculostomy
- Multicompartment hydrocephalus
- Compartmentalized hydrocephalus
- Placement of Ventricular catheter
- Septum pellucidotomy
How is minimally invasive endoscopic neurosurgery done in India?
The method of endoscopic neurosurgery varies widely with the nature of the problem and the location of the target area. In some cases tiny incisions are needed whereas for some approaches there is absolutely no incision needed.
In the case of a pituitary tumour, for example, the endoscopic approach is through a nostril, hence no cut or incision is needed. The neurosurgeon uses a tiny endoscope, only 2.7 mm wide and 20 cm long. The endoscope is maneouvred into the skull base area and provides dramatic, close up images. The resolution of these images is truly sharp and enables the neurosurgeon to make very accurate decisions in terms of affected vs. healthy tissue. These images are truly a generation ahead of the traditional imaging that was possible through microscopes which permitted only external viewing from a distance with its attendant limitations. Micro-surgical instruments inserted through the same nostril are then used to excise the affected tissue. The magnified imagery makes it possible to remove all the affected tissue that is visualised.
What are the advantages of endoscopic brain surgery in India compared to open brain surgery?
As observed above, some neuroendoscopic surgeries do not require any incisions at all. Even in those cases where incisions are required, these are normally the size of a small coin. As compared to this, open brain surgeries involve long incisions and deep cuts in the body tissue. The consequent trauma can quite often result in complications by way of infections, loss of brain function, etc. All these difficulties are eliminated by the use of neuroendoscopic surgery.
In view of the minimal tissue damage caused by neuroendoscopic surgery in India, it is now also possible to offer treatment to several patients who may earlier have been ruled unfit for open brain surgery on account of age or other medical conditions.
Neuroendoscopic surgery in India also brings down dramatically the duration of hospital stay required by patients. Most patients are able to leave the hospital within a day or two after the surgery. Along with attendant reductions in cost, this also minimises the chances of patients acquiring hospital-stay related infections.
Do hospitals in India perform endoscopic neurosurgeries?
Our associate hospitals in India do perform a wide range of endoscopic neurosurgeries. These hospitals are equipped with the latest in terms of diagnostic equipment, such as Brain Suite as well the latest neuro endoscopic surgery equipment.

There are several neurosurgeons in India who have specifically trained abroad in the latest neuro endoscopic surgery techniques and have performed a large number of procedures both in the West and in India.
×
Stereotactic Radiosurgery in India
What is Stereotactic Radiosurgery?
Stereotactic Radiosurgery, contrary to the way it sounds, is not an invasive surgery. It is a non-invasive procedure that uses high-powered x-rays or gamma rays in a very focused manner on a precisely defined portion of the body. This procedure has been used to treat brain disorders for several years but Stereotactic Radiosurgery in India is now finding application in treating medical conditions in other parts of the body such as the lung, liver abdomen, prostate, head and neck as well.
What medical conditions are treated by Stereotactic Radiosurgery in India?
Stereotactic Radiosurgery is being effectively used to for the treatment of several tumours in the brain and in the nervous system. A few examples:
- benign and malignant tumours in the brain and the spinal cord
- primary and metastatic tumours in the brain and the spinal cord
- tumours in the pituitary region
- head and neck cancers
- acoustic neuroma
- AVM ( arteriovenous malformations)
- epileptic disorders
- Deep Brain Stimulation (for Parkinson's Disease)
- Trigeminal Neuralgia
When is Stereotactic Radiosurgery a better option?
Invasive surgery is not an option in those cases where the tumour or the target sites:
- are inaccessible ( for example, deep seated brain tumours)
- are very proximate to important nerves or vital organs (with the consequent possibility of significant collateral damage in the course of doing invasive surgery)
In the above situations, stereotactic radiosurgery in India is a good option to consider.
- Identification of the tumour, its exact location shape and size: Three-dimensional imaging techniques are used to identify the precise details of the tumour that is to be targeted. CT, MRI and PET-CT are the modalities used in the planning process
- Immobilisation of the targeted body region: Specially designed devices are used to ensure that that the tumour location does not change on account of physical movement by the patient of the targeted part of the body, for example the head.
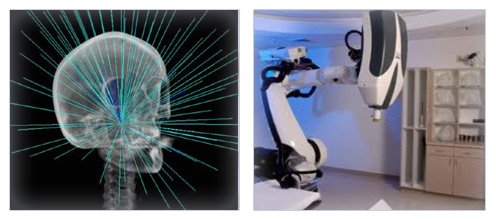
- Radiation delivery to the target site: Highly focused and powerful gamma or x-ray beams are trained on the target site from multiple angles. For some disorders, one single session of radiation delivery is sufficient. For some other situations, where the tumour is larger than 2.5 cm, radiation is delivered over four or five sessions. This method is called Fractionated Stereotactic Radiosurgery.
The delivery of radiation to the target site is typically done by using Linear Accelerator (LINAC) machines which are widely available at our associate hospitals in India. Some of our associate hospitals in Delhi, Mumbai, Bangalore, Chennai and Hyderabad also have the latest generation LINAC machines ( Novalis Tx, CyberKnife, etc). These machines deliver photons (x-rays at very high energy levels) to the tumour site in a very precise manner.
Radiation delivery is also done using the Gamma Knife which uses gamma rays instead of x-rays. The Gamma Knife surgery in India is considered to be more useful in the treatment of small tumours, while LINAC machines can handle large tumours as well.
How is Stereotactic Radiosurgery done in India?
Stereotactic Radiosurgery comprises the following steps:
- Identification of the tumour, its exact location shape and size: Three-dimensional imaging techniques are used to identify the precise details of the tumour that is to be targeted. CT, MRI and PET-CT are the modalities used in the planning process
- Immobilisation of the targeted body region: Specially designed devices are used to ensure that that the tumour location does not change on account of physical movement by the patient of the targeted part of the body, for example the head.
- Radiation delivery to the target site: Highly focused and powerful gamma or x-ray beams are trained on the target site from multiple angles. For some disorders, one single session of radiation delivery is sufficient. For some other situations, where the tumour is larger than 2.5 cm, radiation is delivered over four or five sessions. This method is called Fractionated Stereotactic Radiosurgery.
The delivery of radiation to the target site is typically done by using Linear Accelerator (LINAC) machines which are widely available at our associate hospitals in India. Some of our associate hospitals in Delhi, Mumbai, Bangalore, Chennai and Hyderabad also have the latest generation LINAC machines ( Novalis Tx, CyberKnife, etc). These machines deliver photons (x-rays at very high energy levels) to the tumour site in a very precise manner.
Radiation delivery is also done using the Gamma Knife which uses gamma rays instead of x-rays. The Gamma Knife surgery in India is considered to be more useful in the treatment of small tumours, while LINAC machines can handle large tumours as well.
How does Stereotactic Radiosurgery work?
Stereotactic Radiosurgery in India works by damaging the DNA of the tumour cells. Cancers are primarily caused by abnormal cells that multiply rapidly. Radiation, by damaging the DNA of the cells, neutralises their ability to multiply. Thus, over a period of time, the tumour size shrinks. Malignant tumours shrink fairly rapidly while benign tumours take a longer time, sometimes even a couple of years.
Who are the specialists involved in conducting Stereotactic Radiosurgery in India?
Treatment using Stereotactic Radiosurgery involves a team of specialists:
- the neurosurgeon who is primarily in charge of the patients treatment
- the radiologists who read and interpret the CT, MRI and PET-CT images
- the radiation oncologist who defines the entire radiation plan (target definition, radiation dose definition and overall treatment plan)
- the radiation physicist who along with a dosimerist calculates radiation dosages and the specifics of radiation delivery
- the radiation therapist-technician who operates the machine, positions the patient, etc
Does this procedure involve hospitalisation?
Hospitalisation is not essential. However for our foreign patients visiting India for treatment, it is more convenient to have the patient admitted to the hospital for two to three days, so that imaging and workup of the patient can be conducted rapidly and comfortably with the patient within the hospital.
Patients are normally able to resume normal activity within a day or two of the procedure.
×
Ventriculoperitoneal (V P) shunting for
hydrocephalus in India
What is coronary angiogram (also known as cardiac catheterization)?
A coronary angiogram, also known as cardiac Cath or cardiac catheterisation, is a minimally invasive diagnostic procedure that is widely used for invest igating heart disease, a common medical problem in India. It enables the interventional cardiologist to visualise the functioning of the heart. A catheter - a narrow, flexible tube- is inserted into a blood vessel, normally at the groin or at the wrist, and guided to the heart. The cardiologist is able to see the movement of the catheter as it is threaded towards the heart, by sharp images which are projected by a series of x-rays that are being continuously taken. The procedure yields very clear images of the heart valves, the coronary arteries and the chambers of the heart.
What is the VP shunt?
The VP shunt is a commonly performed neurosurgical procedure in India for the treatment of hydrocephalus, a condition in which there is a buildup of excess pressure within the brain. This procedure aims to transfer excess fluid from within the brain to either the abdominal cavity or the chest region of the body. The transfer of this excess fluid normalises the intracranial pressure (pressure within the brain)
The shunt system consists of two catheters and a valve, both of which are embedded within the body and not visible from the outside.
Some details about hydrocephalus...
The human brain produces about half a litre (500 ml) of cerebrospinal fluid, also known as CSF, every day. This fluid circulates within the brain, acting as a cushion and also supplying nutrients to brain tissue. The generation of the cerebrospinal fluid and its absorption/evacuation is normally equivalent, leading to constant pressure within the brain.
The CSF circulates out of cavities in the brain, called the ventricles, bathing the brain and the spine, and is then reabsorbed by the bloodstream.
Hydrocephalus happens when there is an excess of cerebrospinal fluid within the brain, either on account of an obstruction which prevents the fluid from draining out or if there is a lack of absorption of the cerebrospinal fluid by the bloodstream. Irrespective of the cause, the excessive quantum of the fluid leads to increased pressure within the brain. This leads to decreased brain function and in the long-term, damage to brain tissue.
Types of hydrocephalus
Hydrocephalus can be of the following types:
Communicating hydrocephalus, in which there is no obstruction in the flow of CSF, but there is a lack of absorption of the fluid back into the bloodstream
Non-communicating hydrocephalus, in which the drainage of the CSF out of the brain faces an obstruction, for example, by a tumour
Adult communicating hydrocephalus, also known as Normal Pressure Hydrocephalus (NPH), which occurs in adults. The cause for this condition is often not identifiable. Secondary NPH has been associated with the occurrence of, or following, brain trauma, meningitis, brain haemorrhage, etc.
How is the VP shunt done in India?
The neurosurgeon drills a tiny hole through the skull and inserts a catheter into the ventricular cavity of the brain. The catheter is a synthetic tube that is strong and supple, measuring less than a quarter of an inch. A second catheter is inserted behind the ear and moved down to the abdominal cavity. A one-way valve is placed behind the ear and both the catheters are connected to the valve. The valve is so designed that upon the intracranial pressure reaching a certain level, on account of CSF buildup, the valve opens and allows the CSF to drain into the abdominal cavity. Once the pressure within the brain is normalised, the valve closes again. Our associate hospitals in India also offer magnetic programmable valves, whose settings can be calibrated by the neurosurgeon externally without having to perform another surgical procedure.
Our neurosurgeons in India also perform venous shunts, in which the excess CSF fluid is drained into the chest region. In this case Percutaneous Minimally Invasive Surgery procedure is offered.
Why is a spinal tap done before doing VP shunt in India?
In the case of patients suffering from NPH, the neurosurgeon will perform a spinal tap to draw out some cerebrospinal fluid. This minor procedure in effect simulates the VP shunt procedure.
The measurement of intracranial pressure before the spinal tap and after the spinal tap will provide a very clear indication about the likely outcome, if a VP shunt procedure were to be performed.
What is the prognosis after VP shunt in India?
In general, VP shunts are extremely successful in bringing down intracranial pressure. However it is also important to note that in conditions wherein the hydrocephalus is caused by conditions such as a tumour, meningitis, spina bifida, etc the prognosis will not be comparable.
Is the VP shunt procedure done in hospitals in India?
Yes, the VP shunt procedure is commonly done by the neurosurgeons at our associate hospitals across India with success rates on par with international benchmarks.